Leveraging Technology to Recruit the Right HCPs and HCOs for Clinical Trials

Clinical trials don’t start with patient recruitment. They start with recruiting the right healthcare professionals (HCPs), healthcare organizations (HCOs), investigators and research sites, investigators and research sites, all of which can make or break a study.
If a trial is placed at the wrong sites, with the wrong investigators, everything else becomes harder. Enrollment slows. Data quality suffers. Timelines stretch. Costs rise.
Finding the right HCPs and HCOs for clinical trials involves ensuring they have the appropriate expertise and patient demographics. This can be a complex process, as it requires meeting specific medical criteria and considering geographical factors.
With AI, real-world data, and predictive analytics, it is now possible to identify, engage, and onboard the right HCPs and HCOs faster and more precisely than ever before.
Let’s explore how technology is changing HCP and HCO recruitment, solving common challenges, and making sure trials are placed at the best sites possible.
Challenges in Recruiting HCPs and HCOs for Clinical Trials
In a clinical trial, an investigator is a medical professional, responsible for conducting the study at a specific site. They oversee participant safety, ensure the trial follows protocol, and collect accurate data. Finding the right investigators and research sites is one of the biggest challenges in clinical trials.
Furthermore, finding qualified healthcare professionals (HCPs) and healthcare organizations (HCOs) for clinical trials is a critical yet complex process. Traditional recruitment methods often fall short, creating obstacles that can delay studies and limit patient access to innovative treatments. Traditional recruitment methods—like manually searching through outdated databases, relying on word-of-mouth referrals, and conducting slow, paper-based outreach—often fall short. These inefficiencies can lead to delays in trial timelines, a mismatch between sites and patient populations, and ultimately hinder access to innovative treatments for those who need them most.
Let’s take a closer look at some of the reasons why these traditional methods can pose challenges when conducting clinical trials:
1. Awareness & Engagement Gaps
Many HCPs and HCOs don’t actively seek out clinical trials. They’re focused on patient care, overburdened with administrative work, and are often unaware of ongoing studies that could benefit their patients.
2. The Administrative Burden
Even when HCPs are interested, the paperwork and regulatory requirements can discourage participation. Managing patient eligibility, consent forms, and data submission adds to their already-heavy workload.
3. Misalignment of Patient Populations
In a clinical trial, a sponsor is the individual, company, institution, or organization responsible for initiating, funding, and overseeing the study. Sponsors often struggle to find sites and physicians with the right patient demographics. A trial might need participants with rare genetic markers or different backgrounds, but most recruitment efforts are too broad and inefficient.
4. Slow, Inefficient Screening Processes
Traditional recruitment relies on manual patient screening, which can be time-consuming and prone to errors. This means that if the right patients aren’t identified quickly, trials get delayed
5. Diversity & Representation Challenges
Historically, clinical trials have underrepresented minority groups and patients from rural areas. Recruiting a diverse patient pool starts with recruiting diverse HCPs and HCOs, yet some industries may struggle to do so effectively.
For clinical trials to succeed, sponsors need a better, data-driven way to recruit HCPs and HCOs.
How Technology Enhances Clinical Trial Recruitment
Technology is addressing these challenges by helping sponsors select, vet, and onboard the right HCPs and HCOs more efficiently.
1. AI-Powered HCP & HCO Matching
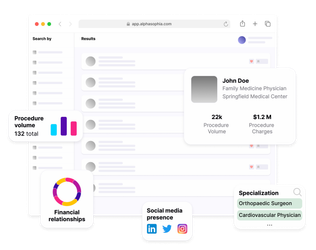
Instead of manually searching through outdated investigator lists, AI-driven platforms like Alpha Sophia can help:
- Identify investigators with expertise located in specific territories with ease.
- Narrow down HCPs by taxonomy, CPT billing codes, billing trends and more, to find suitable HCPs for clinical trials.
- Understand the unique attributes of every physician through detailed profiles.
By using AI and machine learning-powered tools, sponsors can predict which sites will perform best for a specific study, thereby reducing trial delays and optimizing resource allocation.
2. Electronic Health Records (EHR) Integration
A major reason trials fail is that sponsors pick sites without verifying if they have the right patients. Platforms that integrate with electronic health records (EHRs) and insurance claims data help sponsors:
- Match trial criteria with actual patient populations at an HCO before selecting the site.
- Ensure diversity by identifying HCPs serving underrepresented communities.
- Reduce recruitment bottlenecks by ensuring patient access before the study begins.
Instead of relying on assumptions or past trial history, sponsors now have real-time patient data to validate site selection decisions.
3. Digital Outreach & Engagement Tools
Finding the right HCPs is one thing, getting them interested and engaged is another. Many investigators don’t have time to search for new trial opportunities, and traditional outreach methods (cold emails, phone calls) often go ignored.
AI-driven engagement tools help by:
- Analyzing HCP research activity, online publications, and professional networks to identify those most likely to be interested.
- Automating personalized outreach based on an HCP’s specialty, past trial participation, and patient demographics.
- Streamlining onboarding with digital contracts, e-consent, and automated regulatory documentation.
This makes the recruitment process more efficient, reducing friction and improving investigator engagement.
4. Predictive Analytics to Avoid Site Overload & Optimize Trial Placement
One of the biggest problems in clinical trials? Selecting sites that are already running too many studies.
Predictive analytics tools:
- Assess current site workload to avoid HCOs that are overburdened with multiple trials.
- Measure past enrollment speed to identify which sites recruit patients efficiently.
- Flag trial competition at an HCO so that sponsors aren’t placing multiple studies that compete for the same patient population.
Instead of blindly selecting sites based on past success, sponsors can balance trial placement based on real-time capacity.
Improving Diversity in Patient Recruitment
Diversity in clinical trials is not only an ethical issue but also a huge scientific necessity. Drugs and therapies need to work across different populations, yet minority groups and underserved communities remain underrepresented in research.
But technology can help close this diversity gap with:
1. AI-Driven Demographic Targeting
AI helps identify HCOs and physicians serving underrepresented populations. Instead of relying on traditional academic centers, sponsors can partner with community clinics and telehealth providers to access a broader patient pool.
2. Digital & Social Media Recruitment
Many patients don’t hear about clinical trials from their doctors. Digital recruitment tools like Facebook Ads, Google search campaigns, and online patient registries help reach different sections of the population where they are already active online.
3. Wearable & Mobile Health Tech
Devices like Fitbits, Apple Watches, and remote monitoring apps allow patients to participate in trials without frequent hospital visits. This removes a major participation barrier for underserved groups.
Ensuring the Right Patient Demographics Through HCP and HCO Selection
Sponsors need partners who:
- Have access to the right patient populations
- Are experienced in trial protocol compliance
- Can efficiently manage recruitment & retention
Using data-driven site selection platforms, sponsors can evaluate:
- Patient demographics & health records
- Past trial performance metrics
- Enrollment speed & retention rates
All of this together reduces the risk of selecting underperforming sites and improves trial success rates.
Ethical & Regulatory Considerations in HCP and HCO Recruitment
Technology makes recruitment more efficient, but it also introduces new responsibilities.
1. Data Privacy & Security
AI-driven recruitment must follow HIPAA, GDPR, and other global data privacy regulations when analyzing patient and investigator data.
2. Informed Consent
As recruitment shifts online, sponsors must ensure patients fully understand trial risks and benefits. Digital consent tools (e.g., Medable and Science 37)) use videos, quizzes, and interactive modules to enhance understanding.
3. Avoiding Algorithmic Bias
Site selection tools should be trained on diverse datasets to prevent racial, geographic, or socioeconomic bias in investigator recruitment.
FAQs
1. Why is selecting the right HCPs and HCOs critical for clinical trials?
They ensure accurate patient recruitment, protocol compliance, and reliable data collection, which are key factors in trial success.
2. How does technology improve HCP and HCO recruitment?
AI, EHR integration, and digital outreach streamline the process, making recruitment faster and more targeted.
3. What role does data analytics play in HCP and HCO selection?
It helps identify high-performing sites with the right patient populations, reducing trial failures.
4. Can technology help improve diversity in clinical trials?
Yes. AI targeting, digital recruitment, and telemedicine expand access to underrepresented groups.
5. How do AI and predictive modeling enhance clinical trial recruitment?
They analyze large datasets to identify ideal sites, physicians, and patients, improving speed and efficiency.
Conclusion
Traditional methods of recruiting HCPs, HCOs, and patients aren’t efficient enough for modern clinical trials. AI, digital platforms, and EHR integrations are helping to reduce trial timelines, improve patient diversity, and ensure high-quality recruitment.
So, sponsors who adapt their recruitment strategies with technology will see stronger, faster, and more cost-effective trials.
Recruit the right HCPs and HCOs with Alpha Sophia