Rethinking KOL Strategy in 2025: Why Influence Looks Different Post-Pandemic

The world of Key Opinion Leader (KOL) engagement has undergone a profound shift. In 2025, medical affairs teams are no longer asking who the top voices are in theory—they’re asking who’s actually shaping clinical behavior on the ground.
The legacy approach to KOL strategy—relying heavily on academic standing, publication volume, or speaker bureau presence—is giving way to a more nuanced, data-driven model of influence. The pandemic only accelerated this transition. Clinical decision-making moved into decentralized, digital-first environments. Peer influence became more distributed. HCPs who once shaped practice by lecturing at congresses are now joined—or in many cases, outpaced—by frontline clinicians, digital-native educators, and peer connectors within referral networks.
This evolution in influence demands a full strategic reset. What worked in 2015 won’t cut it in 2025. And teams that cling to outdated models risk wasting resources on the wrong relationships—and missing the clinicians actually moving the needle.
Start Your Omnichannel Strategy with Alpha Sophia
From Anecdotes to Analytics: Redefining What Influence Means
For decades, KOL identification was guided by a well-worn rubric:
-
Number of publications
-
Number of conference presentations
-
Academic or hospital affiliation
-
Role in guideline panels or societies
This framework worked when influence was centralized. When large academic centers dominated innovation. When the same voices surfaced in journals, podiums, and advisory boards.
But in a fragmented and fast-moving healthcare system, those proxies are no longer enough. Modern influence is contextual, localized, and often invisible on PubMed.
Today’s influential physicians may not be publishing—but they’re performing thousands of high-impact procedures annually. They may not be speaking at every congress—but they’re active in specialty societies, shaping discussion via WhatsApp groups, Slack channels, or regional panels. And they’re often the people other clinicians turn to for peer input in real time.
To find them, you need data. Not anecdotes. Not Rolodexes. Real-world clinical behavior, referral patterns, and network insights.
Three Core Pillars of Modern Influence Mapping
Let’s break down what a modern KOL profile looks like in 2025—and what data supports that visibility:
1. Clinical Throughput
Procedure and claims volume are critical indicators of frontline impact. If a clinician consistently ranks in the top decile for your relevant CPT or ICD-10 codes, they are shaping clinical pathways—regardless of whether they’re speaking at congresses.
Granular claims data (like CMS Part B or commercial all-payer feeds) reveals the physicians treating your exact patient population. This becomes particularly valuable in underserved geographies or community settings where traditional KOLs have limited reach.
2. Network Centrality
It’s not just about what a physician does—it’s who they influence. Network analysis tools can identify “connectors”: clinicians with a high degree of patient-sharing, referral activity, or peer visibility. These individuals can shape local consensus far more effectively than top-line names with minimal real-world ties.
Studies have shown that patient-sharing networks strongly correlate with clinical adoption trends and even prescribing quality. A physician with strong local referral ties may influence dozens of providers indirectly.
3. Scholarly and Digital Footprint
Publications still matter—but only as part of a larger story. Abstracts, congress involvement, social media visibility, and community-level education activity all feed into a holistic view of influence. This is where next-generation data platforms make a difference: by merging these sources into single HCP profiles with trackable scoring.
Also important: visibility into Open Payments history and historical honoraria, which help screen for potential conflicts or fatigue from previous overuse.
Every US physician at your fingertips. Always.

Why This Matters: The High Cost of Getting KOL Strategy Wrong
Advisory boards, MSL engagement, and educational programming all hinge on getting the right people in the room. And in 2025, that room is changing fast.
A misaligned KOL strategy leads to:
-
Overpayment for underperformance
-
Redundant messaging to disengaged stakeholders
-
Missed insight from actual decision-makers
-
Poor ROI on scientific exchange efforts
It also poses compliance risks. Regulators increasingly scrutinize honoraria payments under the lens of “fair market value” (FMV). Without clear rationale tied to real-world data, those justifications fall flat.
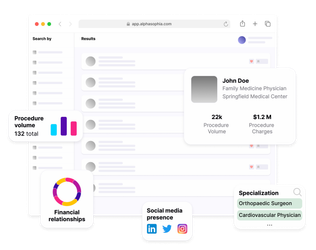
How Alpha Sophia’s Data Supports This Shift
This new era of KOL mapping requires infrastructure—especially for lean or growing medtech companies that don’t have a full-time analytics team.
That’s where platforms like Alpha Sophia subtly enable this shift:
-
Claims data ingestion helps teams understand clinical volume by diagnosis or procedure
-
Network analysis surfaces peer-connected HCPs, not just podium speakers
-
PubMed and congress scraping highlights scholarly activity, even for non-headliners
-
Open Payments integration ensures compliant and balanced panels
-
Scoring engines allow for weighted, transparent selection of targets across different strategies (e.g., market access vs. education vs. protocol development)
Instead of 12 spreadsheets and guesswork, you get a centralized, audit-ready way to build panels, assign MSL outreach, and segment HCPs by actual influence.
Want to build an advisory board that reflects this thinking? Read: Using Healthcare Data to Build Better Advisory Boards →
Implications for MSLs: Precision Over Presence
Medical Science Liaisons are at the front lines of this shift. Their success depends not just on building relationships—but building them with the right people.
That means:
-
Narrowing outreach to high-opportunity clinicians
-
Customizing materials based on prior procedure volume or engagement
-
Capturing and feeding insights back into broader strategy
When powered by integrated profiles that update quarterly, MSL targeting becomes both proactive and efficient. Instead of blanket coverage, reps can prioritize 20 HCPs who will actually shape protocol or adoption, while still maintaining broader awareness of emerging players.
Also read: The New Rules of HCP Activation: Building Trust at Scale →
From One-Off Tactics to Ongoing Intelligence
The best KOL strategies in 2025 don’t stop at identification. They’re cyclical and data-powered.
That means:
-
Continuously updating tiers based on real-world impact
-
Measuring outcomes from advisory meetings or slide deck input
-
Revising strategies quarterly based on shifting networks or claims data
-
Using CRM-integrated dashboards to track who’s been touched, when, and why
It’s no longer acceptable to build a speaker bureau once a year and call it a day. Influence is dynamic. So your tools—and your workflows—have to match.
Final Thought: KOL Strategy is Now a Data Strategy
We’re in a new era. Influence can no longer be inferred. It must be proven. And that means your KOL strategy needs to be backed by the same rigor, data, and systems you’d apply to market access or regulatory planning.
The stakes are high. If you want to compete, your team must stop relying on past lists and gut feel—and start leaning on the data.
In this environment, the difference between a good KOL program and a great one isn’t how many people you reach—it’s how well you choose the ones who matter.
