Top 10 Healthcare Trends in 2025: What’s Changing and Why It Matters

Healthcare in 2025 is not what it used to be five years ago. The industry is moving beyond traditional care models, driven by new technology, shifts in patient expectations, and a greater emphasis on efficiency and accessibility.
If you’re part of this ecosystem, understanding these emerging trends will help you stay ahead. Let’s break down the top trends transforming healthcare this year and why they’re important.
Precision Medicine
For years, healthcare has operated on a generalized approach. If a treatment works for most people, it’s considered a success even if it fails for 30% of patients.
Precision medicine is putting an end to that by using genetic data, environmental factors, and lifestyle insights to make treatments customized for each patient. This is most visible in oncology, where therapies like targeted monoclonal antibodies are designed to attack cancer cells with pinpoint accuracy based on a patient’s genetic mutations. It was once reserved for cutting-edge labs and is now entering mainstream clinics.
Such a change matters because it drastically improves outcomes. A patient undergoing precision-targeted chemotherapy is far more likely to avoid unnecessary side effects than one on a generalized regimen.
For healthcare systems, it also means significant cost savings, as resources aren’t wasted on ineffective treatments.
Telehealth Expansion
Telehealth refers to the use of digital information and communication technologies, such as computers and mobile devices, to deliver and manage healthcare services remotely. Telehealth is no longer a secondary option; it’s the first point of contact for many patients. The pandemic accelerated its adoption, but in 2025, telehealth has matured into a comprehensive ecosystem. Virtual consultations, remote monitoring, and even virtual physical therapy are now mainstream.
For rural communities, this means unprecedented access to specialists. For urban centers, it reduces wait times and frees up in-person appointments for critical cases. However, telehealth’s real impact lies in chronic disease management.
A patient with hypertension might wear a device that tracks their blood pressure in real-time, sending data directly to their care team. Instead of waiting for a crisis, providers can intervene early.
While it’s been a blessing for urban and suburban areas, rural and underserved populations often lack the broadband infrastructure necessary to participate fully.
Artificial Intelligence Integration
Artificial intelligence has quietly embedded itself into the healthcare system, and its presence is only growing. In diagnostics, AI tools analyze mammograms, CT scans, and pathology slides with unprecedented accuracy, often catching anomalies that even experienced clinicians might miss.
In operations, AI optimizes workflows, from patient scheduling to supply chain management, reducing inefficiencies and freeing up resources.
But perhaps the most exciting development is predictive analytics. AI can analyze a patient’s health records and flag those at risk of conditions like sepsis or heart failure.
Hospital-at-Home Programs
Few trends highlight the changing face of healthcare as dramatically as hospital-at-home programs. Advances in technology allow patients to receive acute care like IV antibiotics, oxygen therapy, and even advanced diagnostics without ever setting foot in a hospital.
Studies also show that patients recovering at home have lower rates of hospital-acquired infections and better overall satisfaction.
For hospitals, the benefits are equally compelling. With beds often at capacity, offloading less critical patients to home-based care frees up resources for those who truly need them. But, scaling hospital-at-home programs needs robust infrastructure and a significant cultural shift among providers and patients alike.
Digital Therapeutics
Digital therapeutics (DTx) are software-driven interventions designed to treat or manage medical conditions. For example, platforms helping patients with type 2 diabetes monitor their blood sugar levels or apps that provide cognitive behavioral therapy for anxiety are becoming an integral part of care plans.
These are rigorously tested, FDA-approved solutions backed by clinical evidence. In 2025, DTx will be particularly impactful in managing chronic diseases like diabetes, where tools offer real-time coaching, medication reminders, and even behavior modification programs.
The most striking aspect of it is that while traditional therapy might require physical infrastructure and human resources, DTx can be delivered to thousands of patients simultaneously. This essentially democratizes access, especially in underserved areas.
Mental Health Technology
The demand for mental health services has reached an all-time high, and traditional systems are struggling to keep up. Technology is stepping in to fill the void, with platforms offering virtual therapy, mindfulness apps, and even AI chatbots capable of providing immediate support.
Although these tools are not replacements for therapists, they are crucial bridges for those who might otherwise go without care. For example, an AI platform might provide cognitive behavioral therapy exercises to a patient with mild anxiety, freeing up therapists to focus on more severe cases.
For patients, these tools offer immediate support in a system often plagued by months-long wait times. However, scaling mental health technology still presents a significant cultural challenge. Overcoming stigma and ensuring quality is what will make the difference.
Wearable Health Tech
Wearable health technology has evolved far beyond tracking steps. In 2025, these devices are actively contributing to clinical care. From smartwatches monitoring heart rhythms to glucose monitors sending real-time data to doctors, wearables are giving patients unprecedented control over their health.
For providers, this continuous stream of data is invaluable. It enables early intervention and supports preventative care, which reduces hospitalizations and improves outcomes.
For example, a wearable that detects irregular heartbeats can prompt a patient to seek care before a serious cardiac event occurs. However, as these devices become more prevalent, ensuring their accuracy and protecting patient data remain top priorities.
Sustainable Healthcare Practices
From energy-intensive hospitals to single-use plastics, the healthcare industry contributes significantly to global emissions.
Beyond operations, there’s a growing emphasis on promoting plant-based diets and reducing the environmental impact of medical supply chains. Today’s consumers are more eco-conscious than ever, and they expect the same from their healthcare providers.
While these changes can be costly upfront, they often result in long-term savings and improved public trust.
Gut Health Research
The microbiome’s role in overall health is one of the most exciting areas of research today. From digestive health to immunity and even mental well-being, the gut is proving to be central to many processes.
Personalized probiotics, microbiome-focused diets, and targeted therapies are helping patients manage conditions like irritable bowel syndrome and autoimmune diseases. While this field is still emerging, the potential for microbiome research to inform preventative care is enormous.
Patient Experience
Patients now expect their interactions with providers to be as seamless and personalized as their experiences with consumer brands. Facilities, like intuitive booking systems and real-time updates on their care plans, are becoming more patient-centric.
Engaged patients are more likely to adhere to treatments and make healthier choices, ultimately improving outcomes. For providers, this means investing in tools and training that prioritize communication, transparency, and convenience.
FAQs
1. What are the medical advances in 2025?
In 2025, breakthroughs include AI-driven diagnostics, precision medicine tailored to genetics, and digital therapeutics for chronic disease management. These innovations improve outcomes, reduce costs, and make care more personalized.
2. How big is the healthcare market in 2025?
The global healthcare market is projected to exceed $12 trillion, with digital health—telehealth, wearables and AI, accounting for a significant portion of this growth.
3. What is the future of healthcare in 2030?
By 2030, healthcare will be predictive, personalized, and largely decentralized. AI, nanotechnology, and advanced wearables will dominate, making prevention the primary focus rather than treatment.
4. How will AI impact healthcare in 2025?
AI will revolutionize healthcare by enhancing diagnostics, predicting patient outcomes, and automating workflows. It will improve efficiency, but data privacy and bias remain key challenges.
5. Will telehealth continue to grow in 2025?
Yes, telehealth will expand into chronic care, remote monitoring, and virtual rehabilitation, becoming a core part of healthcare delivery globally.
6. Why is cybersecurity becoming a major concern in healthcare?
With more patient data online, healthcare is a prime target for cyberattacks. Protecting sensitive data and medical devices is critical to maintaining trust and compliance.
7. Will healthcare regulations change significantly in 2025?
Yes, regulations are evolving to address AI ethics, telehealth standardization, and data security. These changes aim to ensure that innovations prioritize patient safety and equity.
Conclusion
These trends are setting the stage for its future. The industry is moving toward a model that is more personalized, accessible, and efficient. However, this transformation comes with challenges.
Providers must balance innovation with ethics, ensuring that advances benefit all patients, not just the privileged few. For stakeholders across the board, the focus should be on creating a system that delivers better care, not just faster or cheaper care.
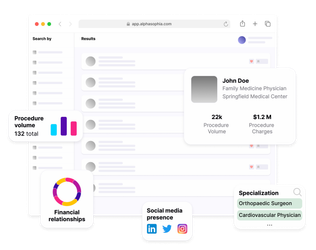
Accelerate product adoption with Alpha Sophia