Top 10 Must-Have Medical Diagnostic Equipment Systems for Modern Healthcare Facilities

A patient walks into your hospital with severe chest pain. The difference between saving their life and losing crucial minutes depends entirely on your medical diagnostic equipment.
Without the right tools, your team is flying blind, unable to detect a heart attack in real time, or failing to catch a growing tumor before it’s too late.
Every hospital, clinic, and diagnostic lab needs modern diagnostic equipment that delivers faster, more accurate results. From MRI scanners to surgical devices, the right tools determine how well you diagnose, treat, and ultimately save lives.
In this article, we’ll break down the 10 essential diagnostic tools every healthcare facility needs and also discuss key considerations when purchasing them.
Top 10 Must-Have Medical Diagnostic Equipment Systems
The accuracy and efficiency of medical diagnostics directly impact patient outcomes. The right equipment shortens time-to-diagnosis, improves treatment planning, and reduces complications, ensuring that healthcare providers make informed decisions when it matters most.
Below are 10 must-have medical diagnostic tools that every facility needs to deliver high-quality, efficient, and data-driven patient care.
1. MRI Scanners
A CT scan will tell you if a patient has a brain tumor. An MRI will tell you where it is, how big it is, and what kind of tissue it’s affecting. That’s the difference.
MRI scanners are non-negotiable if your center handles neurology, oncology, orthopedics, or soft tissue injuries. They provide the highest level of detail for brain abnormalities, spinal cord damage, ligament and tendon tears, and tumor detection.
Unlike X-rays or CT scans, which rely on ionizing radiation, MRI uses magnetic fields and radio waves to create high-resolution, cross-sectional images.
The best facilities are now moving to 3T MRI scanners, which offer twice the magnetic strength of standard 1.5T models. This means clearer images, faster scans, and better precision in detecting small lesions or structural abnormalities.
2. CT Scanners
Every second counts in an emergency room. Unlike MRI, which provides detailed soft tissue imaging but takes longer, CT scans use X-ray technology combined with computer processing to generate cross-sectional images of bones, blood vessels, and internal organs in seconds.
Hospitals handling high patient volumes invest in 128-slice or 256-slice CT scanners, which offer sharper images, faster scans, and lower radiation exposure.
AI-powered CT systems further enhance diagnostics by automatically detecting lung nodules, fractures, and early-stage cancers, reducing human error and diagnosis time.
3. Ultrasound Machines
Ultrasound is one of the most widely used imaging modalities in medicine and for good reason. It’s fast, non-invasive, and radiation-free, making it perfect for cardiac, and vascular assessments and emergency trauma scans.
It’s indispensable in obstetrics, but its role extends far beyond pregnancy. Doppler ultrasound is essential for evaluating blood flow, detecting clots, and assessing vascular health.
The biggest advancements are happening in AI-assisted ultrasound, where real-time image enhancement and automated anomaly detection are reducing operator dependency and interpretation errors.
Meanwhile, handheld wireless ultrasound devices are making high-quality imaging accessible in ambulances, field hospitals, and remote clinics, expanding diagnostic capabilities far beyond traditional settings.
4. X-Ray Machines
Speed is the reason X-rays remain the first-choice imaging tool in emergency and trauma care. Digital X-ray systems have now made imaging faster, clearer, and safer, reducing radiation exposure while delivering instant results.
Portable X-ray units are also changing workflows, allowing imaging to be done at the bedside, in the ICU, or even in ambulances.
The biggest shift is happening with AI-assisted X-ray analysis. Hospitals integrating AI-powered detection software are identifying fractures, tumors, and lung abnormalities faster, reducing reliance on overburdened radiology departments.
5. ECG Machines
No cardiology unit, emergency room, or ICU can function without an ECG machine. It’s the fastest, most reliable way to detect arrhythmias, ischemia, and cardiac abnormalities before they turn into full-blown emergencies.
A standard 12-lead ECG helps physicians diagnose myocardial infarctions, conduction disorders, and hypertrophic changes in minutes. In critical cases, early ECG readings can even mean the difference between timely intervention and irreversible damage.
Cloud-based ECG systems now allow cardiologists to review data remotely, making early detection and continuous patient monitoring possible outside of hospital settings.
6. Blood Pressure Monitors and Pulse Oximeters
Blood pressure (BP) and oxygen saturation are two of the most routinely measured vitals in healthcare, but they’re also among the most critical indicators of a patient’s overall stability.
A hypertensive crisis or a sudden drop in oxygen levels can signal imminent cardiac arrest, respiratory failure, or sepsis, requiring immediate intervention.
Modern BP monitors provide quick, consistent readings, while ambulatory BP monitoring (ABPM) tracks fluctuations over 24 hours, catching hypertension that standard tests miss. Pulse oximeters are now essential in ICUs, COVID-19 care, and post-op recovery, ensuring oxygen levels stay stable.
Portable, wireless models are making remote patient monitoring easier, helping doctors track high-risk cases beyond the hospital.
7. Mammography Machines
Mammography remains the most effective screening tool, identifying tumors before they become symptomatic.
Today’s 3D digital mammography (tomosynthesis) provides sharper imaging, reducing false positives and false negatives, especially in dense breast tissue, where traditional 2D scans often miss abnormalities.
AI-assisted detection is now helping radiologists spot early-stage tumors faster, improving outcomes while cutting unnecessary biopsies.
Facilities are also expanding screening options with Automated Breast Ultrasound (ABUS) for better imaging in high-risk patients, ensuring fewer missed diagnoses and more accurate results.
8. Endoscopy Systems
Gastrointestinal and pulmonary specialists rely on high-definition endoscopes to diagnose and treat conditions earlier. Capsule endoscopy, where a tiny camera is swallowed like a pill, now provides a full scan of the digestive tract without sedation or discomfort, expanding screening capabilities.
AI-powered analysis is improving early detection of abnormalities, helping specialists catch cancerous growths sooner and reduce unnecessary procedures.
9. Point-of-Care Testing (POCT) Devices
POCT devices deliver lab-quality results in minutes, eliminating delays that come with traditional lab testing.
In emergency rooms, ICUs, and primary care settings, rapid tests for glucose, cardiac markers, infections, and coagulation disorders help clinicians make faster, data-driven decisions.
Portable blood analyzers, rapid antigen tests, and handheld electrolyte monitors are now standard in hospitals, reducing turnaround times and improving patient outcomes. Moreover, the integration of lab-on-a-chip technology is making POCT even more precise, allowing for faster detection of sepsis, metabolic disorders, and respiratory infections.
10. Robotic Surgical Systems
Minimally invasive surgery has advanced significantly, and robotic-assisted surgical systems are now redefining precision in the operating room. These systems allow surgeons to perform complex procedures with enhanced control, smaller incisions, and faster recovery times.
Used in urology, gynecology, cardiothoracic surgery, and oncology, robotic systems provide greater dexterity and visualization than traditional laparoscopic tools. AI-assisted robotic platforms now offer real-time tissue analysis, motion scaling, and automated safety features, reducing complications and improving surgical outcomes.
As hospitals adopt robotic-assisted surgery across more specialties, the technology is driving shorter hospital stays, reduced post-op pain, and better patient outcomes.
Key Considerations When Choosing Medical Diagnostic Equipment
Every piece of diagnostic equipment you bring into a hospital affects efficiency, accuracy, and patient care. But the best technology in the wrong setting is a wasted investment. The wrong choice can slow down workflows, produce unreliable results, or add unnecessary costs.
Here’s what healthcare facilities need to evaluate before choosing new diagnostic equipment.
Accuracy & Reliability
Hospitals need equipment that delivers consistent, correct results every time. False negatives in cancer screening or incorrect ECG readings can lead to misdiagnosis and delayed treatment.
Regulatory approvals like FDA, CE, or ISO certifications ensure reliability. Equipment with AI-driven error detection or automated calibration further reduces diagnostic mistakes, improving patient safety and clinical confidence.
User-Friendliness
Advanced technology is worthless if staff can’t use it efficiently. Diagnostic equipment should have an intuitive interface, minimal learning curve, and seamless integration into existing workflows. Complicated systems slow down patient care and increase the risk of user error.
Hospitals prioritize touchscreen controls, automated analysis, and cloud connectivity to streamline operations.
Maintenance and Support
Even the most advanced diagnostic equipment is useless if it’s constantly down for repairs. Hospitals need reliable machines with minimal downtime.
Service contracts, availability of spare parts, and fast technical assistance are critical factors. Equipment with remote diagnostics and predictive maintenance alerts helps facilities prevent failures before they happen.
Cost and ROI
Price alone doesn’t determine value. The real question is whether the equipment justifies its cost over time. You must consider the total cost of ownership, including maintenance, consumables, software upgrades, and staff training.
High-quality equipment may have a higher upfront cost but offers better durability, fewer errors, and lower long-term operating expenses.
Compliance and Safety
Beyond compliance, safety features like radiation dose reduction in imaging systems, automated infection control in endoscopes, and AI-driven error detection help reduce risks for both patients and clinicians.
Investing in certified, well-documented equipment ensures long-term reliability and legal protection.
How Alpha Sophia Helps in Targeting Healthcare Facilities for Diagnostic Equipment Sales
Hospitals don’t buy machines on impulse, most of their purchases are driven by budget cycles, regulatory approvals, and clinical demand. Targeting the wrong facilities wastes time and resources.
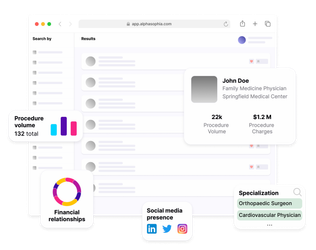
Alpha Sophia helps diagnostic equipment companies target the right healthcare facilities by providing detailed data on which ones are actively purchasing equipment. Instead of wasting time on cold leads, companies can focus on the facilities most likely to buy.
- Alpha Sophia solves this by providing data on healthcare facilities, helping laboratories and diagnostic equipment companies target the right professionals and organizations.
- The platform offers access to valuable data on HCPs and HCOs, with advanced filters such as practice location, taxonomy, procedure codes (CPT, HCPCS), medical society affiliations, and open payments to pinpoint high-volume targets.
- This precision ensures sales efforts are directed towards the most relevant facilities and professionals, optimizing resource allocation, improving outreach efficiency, and boosting conversion rates.
Instead of chasing cold leads, sales teams can focus on high-intent buyers, improving conversion rates and reducing wasted effort.
FAQs
Why is medical diagnostic equipment essential?
It enables early disease detection, accurate diagnoses, and faster treatment decisions, leading to better patient outcomes.
What should hospitals consider when purchasing diagnostic equipment?
Accuracy, ease of use, regulatory compliance, integration with digital systems, and long-term maintenance costs.
How often should medical diagnostic equipment be upgraded?
Most diagnostic tools have lifespans of 5-10 years, but software updates, AI advancements, and regulatory changes may necessitate earlier upgrades.
How is AI transforming medical diagnostic equipment?
AI enhances image analysis, automates diagnoses, predicts disease risks, and improves workflow efficiency, reducing human error.
Conclusion
Hospitals invest in diagnostic equipment to solve real clinical challenges. A purchase only makes sense if it improves accuracy, speeds up workflows, and integrates seamlessly into patient care.
For suppliers, selling is knowing who needs what and when. Alpha Sophia provides real-time insights on facilities actively upgrading their diagnostics, eliminating wasted outreach, and improving sales efficiency.
Accelerate product adoption with Alpha Sophia